Let us help you enhance your efficiency, compliance, and scalability.
Let’s look at where we are today:
CAQH updates handled manually by internal staff
Inconsistent attestation tracking across portals
Delays in payer enrollment impacting revenue cycle
Limited visibility into credentialing status and expirables
High administrative burden on ops
and compliance teams
Are credentialing bottlenecks costing you time and revenue?
We get it. Manual CAQH updates can delay payer enrollment, and missed attestations can cause undesirable reimbursement gaps. We know your internal teams are stretched thin across compliance, onboarding, and billing. Don’t let inconsistent data lead to denials and audit risks.
CAQH is the gateway to payer participation and is required by most commercial payers. This centralized source for provider data drives credentialing timelines, reimbursement eligibility, and network access. Errors or delays can mean lost revenue and provider frustration.
Outsource your CAQH management to dedicated specialists. We’ll handle your profile setup, updates, and attestations, so you can handle the things that really matter.
Outsourcing CAQH management is not just a cost-saving tactic — it’s a strategic move that enhances operation efficiency, compliance, and scalability for provider organizations.
Still not convinced? Let’s look at the perks of outsourcing:
Expertise + Accuracy:
Third-party specialists bring deep knowledge of CAQH workflows, attestation cycles, and payer-specific nuances
Reduce errors and delays that can lead to credentialing bottlenecks or reimbursement gaps
Compliance + Risk
Mitigation:
Attestation compliance is crucial in maintaining healthy payer relationships
Minimize the risk of credentialing lapses, audit finding, or enrollment rejections due to outdated or
missing data
Operational Efficiency + Focus:
Free up internal bandwidth by delegating repetitive, time-consuming tasks, such as profile updates, attestation tracking, and document upload
Allow internal teams to focus on
higher-value activities such as payer negotiations, credentialing strategy, and compliance oversight
Cost-effective Scalability:
Avoid the overhead of hiring, training, and retaining in-house staff for functions that are highly procedural and cyclical
Enable organizations to scale credentialing operations with expanding headcount — especially valuable for multi-state or telehealth groups
Improved Revenue Cycle Performance:
Timely CAQH updates ensure
faster payer enrollment, reducing delays in claims submission and reimbursementSupport clean claims and reduce denials by keeping provider data accurate and aligned across systems
Technology-driven Automations:
Many outsourcing vendors integrate with EMRs, credentialing platforms,
and CAQH APIs to automate data synced and alertsSupport real-time visibility into attestation status, document expirations, and payer-specific requirements
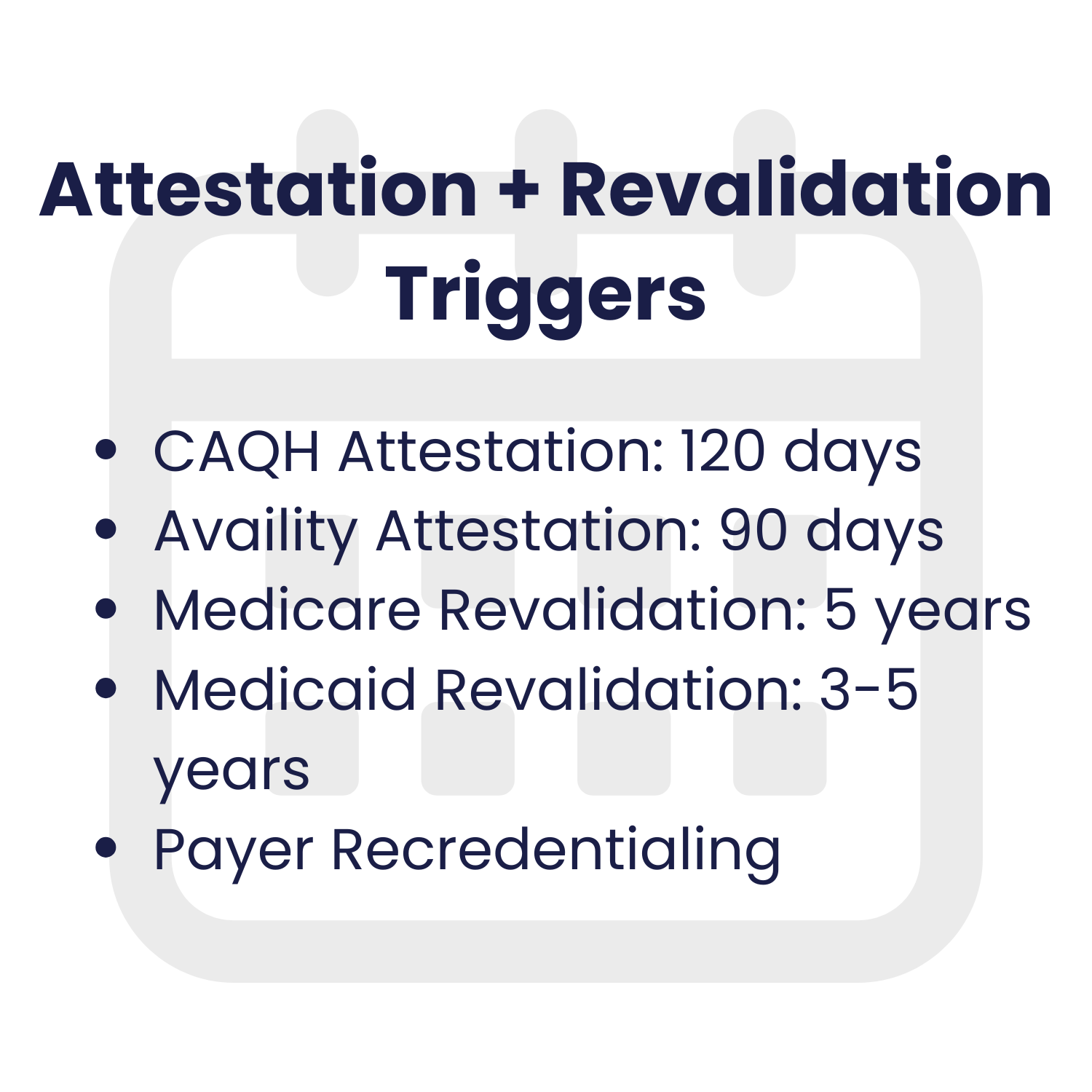
Keeping provider portals current is essential for credentialing accuracy,
payer alignment, and uninterrupted reimbursement.
Here’s a look at some of the key career events that will trigger updates across portals like CAQH, PECOS, NPPES, and
payer-specific systems.